High-cost drugs put valuable employee benefit at risk
Canadian employers face many threats to their bottom line: global competition, an aging workforce, disruptive technologies and more. Perhaps it isn’t surprising, then, that the potential impact of rising drug costs doesn’t get the attention those who track these trends feel it merits. But to attract skilled employees – the foundation of competitive success – employers know they must offer competitive benefits. And in Canada, the most highly valued benefit is the prescription drug plan.
With continued inflationary pressure from new high-cost medications, these plans are at risk, becoming increasingly incompatible with sustainable business models. [Drug Trend Report- Page 69]
Over the last decade, the pharmaceutical industry has responded to the “patent cliff” – the end of price protection for blockbuster drugs such as Lipitor and Zoloft – by focusing their development efforts on high-cost drugs. Without an effective strategic response, this is expected to have an unprecedented impact on Canadian companies and families.
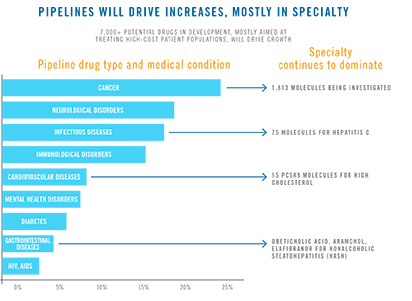
There are currently 7,000 possible new drugs in development, most which are aimed at the treatment of cancer, neurological disorders and infectious diseases. While these drugs will never have the reach of a drug such as Lipitor, illnesses in these categories affect thousands of Canadian employees and their families.
Read: Exorbitantly priced drugs challenge Canadian families, benefit plans
For example, according to the Canadian Cancer Society, about 202,400 people were expected to be diagnosed with cancer in Canada in 2016; about two in five of us are expected to develop cancer in our lifetimes. New drugs are saving lives, transforming fatal diseases into chronic conditions – but in many cases, the costs are astronomical. And there are 1,813 cancer drugs now under investigation. [Drug Trend Report- Page 69]
Also underway is a shift from drugs that could only be administered in hospital – where they are covered by public healthcare plans – to drugs that can be administered at home, transferring the cost burden to employers and patients.
Read: Financial burdens for Canadians with chronic and complex diseases
Cancer drugs are far from the only concern. In 2015, employer-sponsored plan spending on hepatitis C medications tripled due to highly effective, high-cost new treatments. [Drug Trend Report- Page 15] High cholesterol affects 4.9 million Canadians; a new cholesterol-lowering drug known as a PCSK9 inhibitor was introduced in 2015 at a price of $7,600 per year. [Drug Trend Report- Page 16]
So what does an “effective strategic response” look like in the absence of national and provincial policy changes that might limit the cost impact of these new drugs?
As in previous years, the 2015 Drug Trend Report found that one of every three dollars spent by private drug plans is wasted – that is, it does not improve health outcomes. Preventing waste by helping plan members make health and cost-effective decisions is a key part of the solution and will make funding available for new drugs. When employers engage us to give plan members the information and support they need, in the right way and at the right time, we can help decrease spending waste while improving health outcomes.
Pharmacy support is also an essential part of the solution: our research shows that providing proactive care helps members get the maximum benefit from the drugs their doctors prescribe and may prevent the need for more expensive treatments down the road.
Read: See A day in the life of an Express Scripts Canada® pharmacist.
Leading Canadian employers are taking action to get out ahead of these benefit plan threats, putting programs in place that minimize financial risks without diminishing the value of benefits or jeopardizing employee health.
Read: A strategic approach to safeguarding prescription drug benefits
Interested in learning more about our solutions and how we can help? Speak with us today